There is a lot of talk at present about improvements that have been made as a result of the crisis. These changes include the move to remote working, connected teams, practices working together to create “hubs” for patients to be seen in, data sharing between practices and organisation, and systems working together to make decisions based on needs. I am sure there are many others.
As a result, exercises are emerging (often management led) in identifying the changes we want to keep, and even considering how we can take these changes even further.
There is a presumption, it seems, that the changes made in response to the crisis, are somehow “locked in” for the post-covid future. But the reality is of course that change is never that simple. It would be unwise to underestimate the impact the level of recent change has had on individuals, and the discomfort it has caused. A change made in response to a national crisis is very different from a change made in perpetuity. Throw in a bit of conspiracy theory that there is some masterplan to move away from the core general practice model, and it is not hard to understand why holding the gains made so far will be a challenge, let alone building on them.
What do we know about sustaining improvements? Nicola Bateman produced a guide on the sustainability of improvements made back in 2001. The research was based on the sustainability of changes implemented rapidly in an improvement workshop, but there is a useful parallel here to changes made rapidly in general practice in a covid environment.
What she found was that there are 5 ways changes can go:
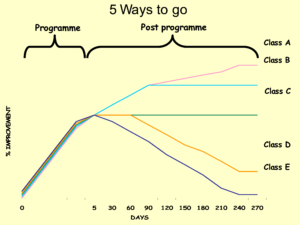
She divided the post programme period into two phases. The first 3 months is primarily concerned with maintaining the new way of working and resolving the technical issues identified during the initial improvement period, and whether these are tackled and resolved.
The Class A and B classifications closed out the actions on the problem follow-up list and maintained the new way of working. Class C maintained the new way of working but failed to close out tasks, and Class D activities closed out the tasks but did not maintain the new way of working. Class E activities failed to do either.
There are lots of interesting lessons in this for us. Beyond understanding that the only way is not up, it highlights that problems identified along the way to making these rapid improvements still need to be tackled and dealt with. According to Bateman, they also need contribution and buy-in from the relevant teams, “making sure that the people who work in the area can contribute to the way in which their area is operated”.
A change implemented out of necessity, steamrollering any resistance along the way, will need engagement of teams to adapt that change to give it a chance of becoming permanent.
Bateman also advises, “ensuring that the team members and their managers remain focussed on the improvement activity”. The idea that remote working (for example) is somehow “done” because it has been going for a few weeks misses the need to be continually addressing issues that arise and adapting it to meet the needs of the practice and its staff. We are not yet at a point where any of the changes we have put in place so far could be considered permanent.
The second phase Bateman divided the post programme period into was from 3 months to 9 months after the initial changes were made. This period is concerned with whether there is any ongoing improvement beyond the initial change period. Class A is what happens when ongoing improvement is in place, as opposed to Class B where there is not.
Being able to make further improvements after these initial gains requires three things: consistency and buy-in; having a strategic direction; and (senior) support and focus. So making the most of the opportunity that seemingly now exists will be no mean feat. It will require a practice to adapt its medium term strategic direction, with full buy-in of the GPs and practice staff, and to develop a clear plan for moving forward.
There are five ways we can go from here. If we are really serious about holding and even building on the gains made in recent weeks then we need to understand there is a lot of work to be done in keeping things as they currently are, let alone taking them beyond the current level.


No Comments