As a GP practice, how do you think of your PCN? Do you see it as a joint initiative between you and your fellow practices to work together to make life better for each other and for your patients? Or do you see it as something you have to do because the GP contract/CCG/government have decreed it?
When you think of the work that does and will take place through the PCN, do you see it as practice work done jointly with the other PCN practices? Or is it “PCN work”, separate from the work you do in the practice?
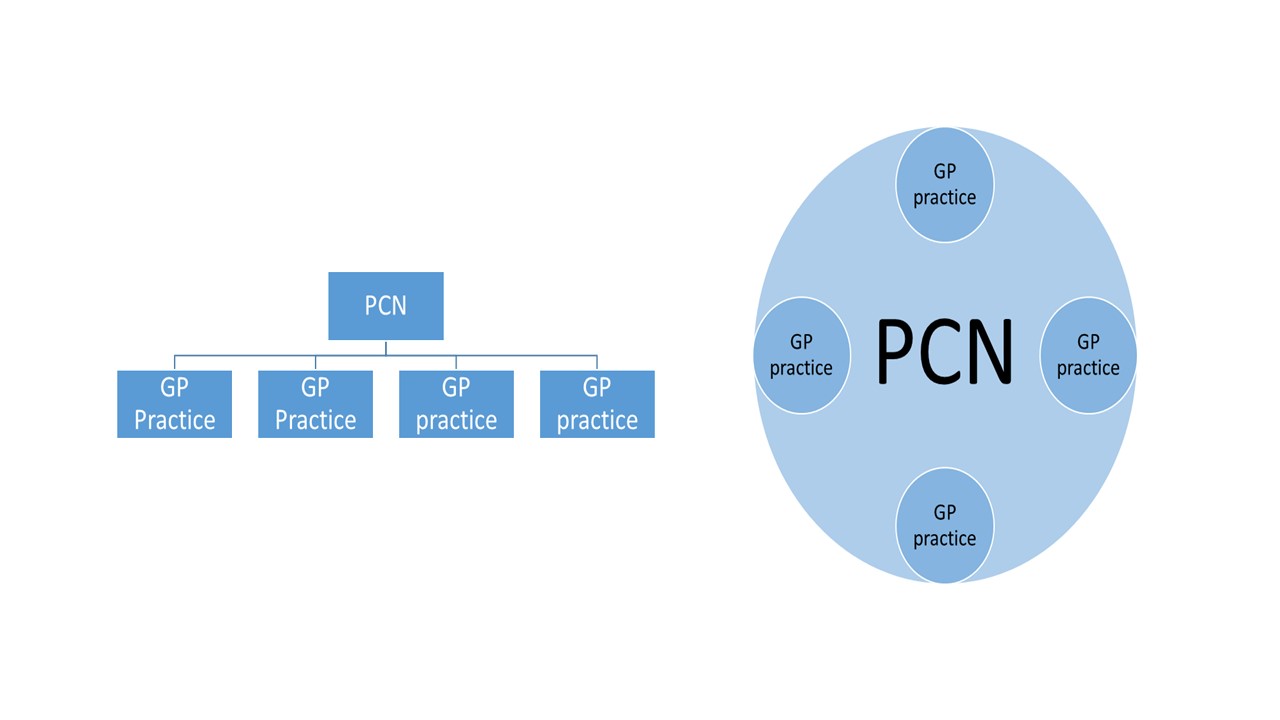
How the relationship with the PCN “feels” to the member practices is crucial. If it feels like the PCN sits above the practices, in a hierarchical fashion (as depicted on the left below), there is going to be a perceived separation between the practices and the PCN. The work of the PCN will feel separate from the “core” work of practices, and the PCN will run the risk of being a burden to practices both in terms of workload and finances.
If the PCN feels like it is the group of practices working together (as depicted on the right), then the opportunity of PCNs for practices is greater. The work of the PCN will support and become part of the core work of practices, rather than operate separately from it. The PCN work becomes the way the practices can improve their workload and their finances.
Even within one PCN the attitude towards it by member practices can vary. You may have one practice viewing it as something separate, but another seeing it as integral to the practice and how it operates. This point was brought home to me this week in a conversation I had with Paul Deffley from Practice Unbound (watch out for this episode of the General Practice podcast coming up in August). He described a pharmacist operating across two practices. It was the same pharmacist following exactly the same processes and seeing exactly the same types of patient.
The reaction to the pharmacist by the two practices was completely different. One practice quickly got to the place where they couldn’t imagine how they ever managed without a pharmacist before, and thought the impact on the GPs and on the practice had been enormous. The other practice was far less enamoured, and if anything thought the pharmacist had created additional work for the GPs. The main difference was the first practice had actively engaged with the pharmacist, invited them to team meetings, and made them part of the practice “family”, whereas the other practice had never embraced the pharmacist in the same way.
If a practice welcomes and takes on the PCN initiatives as part of the way they are now working, the impact for the individual practice, and the for the PCN overall is likely to be considerable. If a practice keeps its focus on what it can control, and keeps the PCN work at arm’s length, the impact will be far less.
The implications of this are huge. It impacts the extent PCNs are able to make changes to meet the needs of practices, and how effectively PCNs can support the sustainability of general practice. It will directly affect the finances. Practices would willingly pay a third of the funding for new services that they want, if the “centre” is chipping in 70%. Subsidising an arms-length PCN initiative for the same amount is an entirely different matter.
It is not the existence of PCNs that is important, but how they operate. This will vary considerably across the country. For all the talk about PCN plans, maturity matrices, and development programmes, my number one focus right now for making a PCN successful would be on getting the relationship between the practices and the PCN right.


No Comments