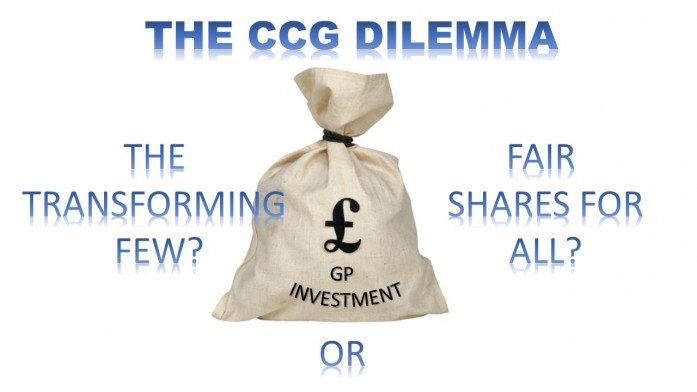
CCGs face a choice. They want to support GP practices to make the changes necessary to get out of their current malaise and to play a more active role in change across the wider system. To do this there are two approaches CCGs can take. Their dilemma is which one to choose.
The first approach is the easiest choice to make. CCGs focus on changes that will impact on all practices. So for example this might be creating incentive systems for practices to get involved in things like managing the complex frail elderly. It may even look like offering services for practices working together, for example to offer extended access. The £3 per head for general practice is divided up evenly for all the practices, and everyone gets their fair share. The proposals are acceptable to the practices, the LMC is happy, and they are deemed equitable by all.
The problem is no actual transformation happens. Practices continue to struggle, emergency admissions continue to rise, and the distance between general practice and the rest of the system does not really change.
The second approach is more challenging to implement. CCGs focus on supporting the small number of practices most likely to drive transformation. They do not make funding and development opportunities available to all. Instead they identify the most dynamic and progressive practices, the ones with a track record of making changes, who are actively seeking to grow, and who have leaders who can make things happen. The CCGs invest in these practices. They ask them what support and resources they need, and they provide it. They work with them to develop solutions that work for general practice as well as the whole system.
It is not an approach that will be popular. The majority of practices will be against it because they will see an uneven share of resources flowing to the “favoured few”. CCG board members whose practices are not part of the selected group will be against it, and they will become representatives of practices who not only are struggling but are now not receiving any further investment. LMCs will be against it because they have a responsibility to represent the wishes of all practices.
But popularity of an approach is not a great indicator of its chances of success. The question for CCGs is do they want the changes in general practice to happen at the pace of the quickest, or the pace of the slowest? The problems in general practice require radical change; changes many practices are not prepared to take. Working with those most likely to make these changes is a far more sensible strategy than it might first appear.
Practices who can make change happen can work with CCGs to overcome the initial resistance. The natural GP leaders are by definition already in these practices. With support they can bring the rest of the practices along. It can still be an inclusive strategy – it just has a different starting point.
The stark reality is the transformation of 7800 GP practices will not happen at the same pace. We are already seeing a small number of practices embracing the need for change and making the most of the opportunities that exist to make themselves fit for the future. But many practices are stuck, unable to find a way forward or to overcome the internal resistance to making the necessary changes. I would argue that hanging on the coattails of those who are moving forward, and focussing support, time and energy into them, is the only approach that will actually deliver results.

1 Comment
Agree that this is a real dichotomy for CCGs. I call it the marmite vs the meringue approach. Spread the marmite thinly over the whole patch and no one can argue it’s not fair. But does everyone like marmite?
Or like a towering meringue build irresistably attractive peak performers?
It may not seem “fair” but if everyone has the same chance to start, it’s their choice. As you quite rightly say, all the innovation adoption theory says the meringues can work, the marmite can’t.