I had butterflies. It was my first day at only my second placement on the NHS management training scheme. I followed the directions I had been given off the motorway and into deepest Salford. The area had long rows of terraced houses interspersed with small corner shops. I passed a group of youths gathered on a corner, hoodies raised, and I hoped they would be out of sight before I had to park and get out of the car. I turned the corner and drove into the car park of an incongruously new and modern building, with immaculate red brick walls and gleaming windows.
It was the Willows Primary Care Resource Centre. It was run by Salford Community Trust; my placement was working with the manager of the new centre. I was excited by the new model of care being implemented here. The centre was based in a district of Salford called Weaste. It was (and I suspect still is) a deprived area, and the centre was part of a community regeneration scheme. The plan was for this centre, which was also home to a GP surgery, to host a range of community facilities, voluntary services and resources, and to act as a “one stop shop” to meet the needs of local people.
An interesting range of services were delivered from the centre. There was a community based leg ulcer clinic, who were using a maggot based treatment for wound care. The Citizens’ Advice Bureau held regular drop-in sessions. There were twice a week art therapy sessions. Physiotherapy and speech and language therapy were provided. Plus there were a whole host of other providers; the space was there, and was available to be used by the local voluntary groups who needed it.
Looking back, and this was over 20 years ago, the model was not hugely dissimilar to the primary care home model. It was serving a defined local population where health and social care needs were closely linked, and it was trying to bring a range of different skills and roles together in one place so that all of the needs of the individuals could be met in one place.
But something was missing. At the time it was hard to put my finger on it. I had a sense of it because sometimes we struggled to attract some of the voluntary groups in to use the centre, and I didn’t really understand why. The locals also seemed to steered clear of the place unless they had a specific reason to attend.
Looking back now, the problem was really one of ownership. The GPs were happy with their new building but by and large left the rest of the centre to others. The district nurses had their base there, but didn’t really interact with the other services running from the centre. Co-location wasn’t resulting in joint working, let alone joined-up care for patients.
The incongruity of the shiny newness of the building with its immediate surroundings meant that rather than local community being proud of it, they were wary and mistrustful. In all the time I was there it never felt like it became the vibrant hub I think was initially intended. Nobody really owned the vision for the place, there was no one driving with a passion to change the lives of the local community. So while the original plans were followed and put in place, it never took off or had the impact that once had been imagined.
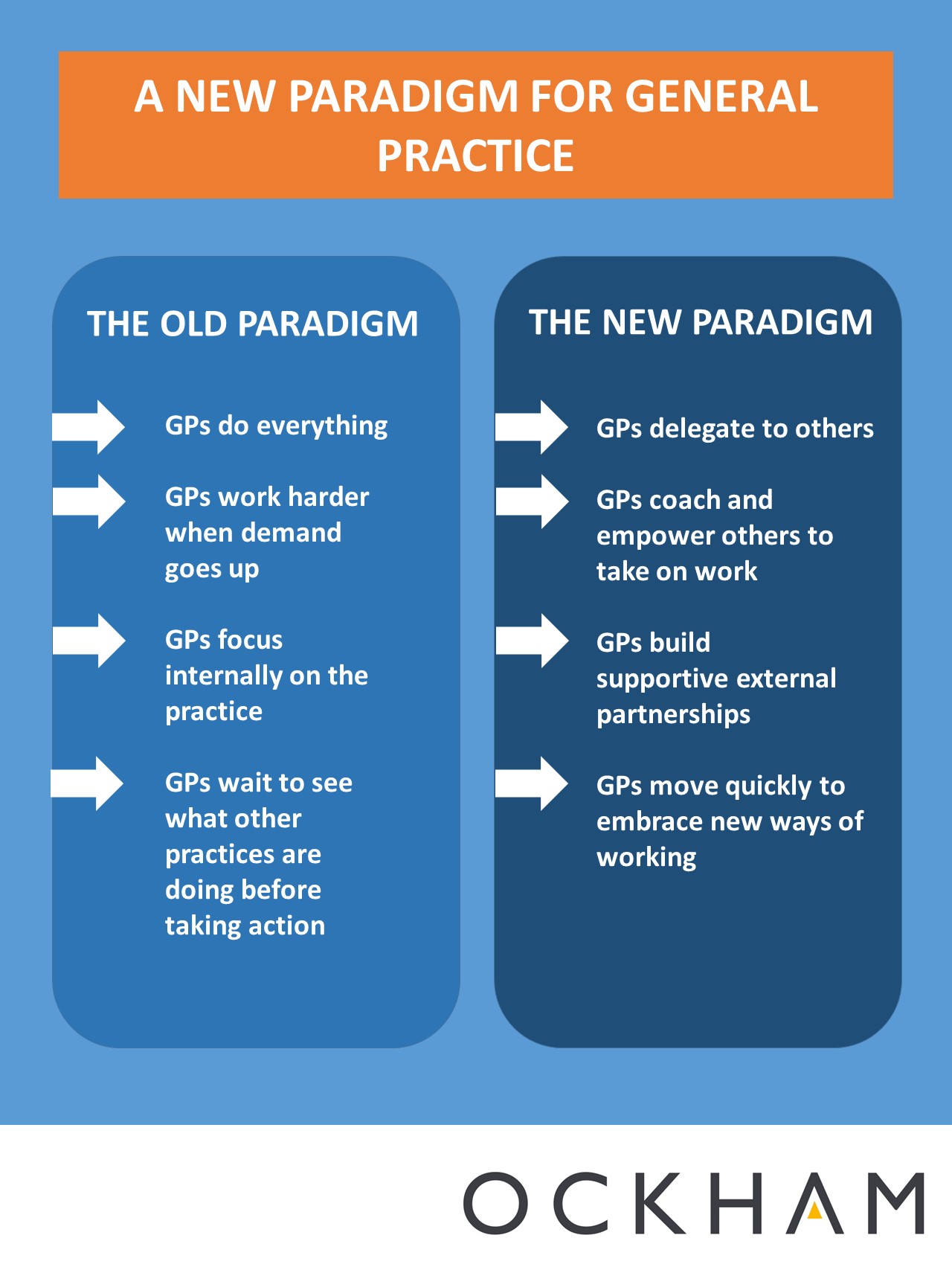
What that whole experience taught me is that however good the “model” is, however well we design it, however shiny the building we put it in, it won’t work on its own. It is all about implementation. Not PRINCE-style implementation. But implementation that is about people, about partnerships and about passion. Implementation that is about leadership from individuals who care. And it needs GPs, community teams and voluntary groups to share a vision for the future, a picture of what can be achieved, and to find a way of partnering with the local population to make it happen.
There was nothing wrong with the primary care resource centre as a model. It was a good model. Equally, there is nothing wrong with the primary care home model. But the model will only ever be one part of the story. It takes people who care and who are prepared to step forward to turn a good model into something that will make a real difference.